BoneChat
What: A new online community built just for Orthopedic Professionals (founded by Tiger Buford).
Why: A safe place to communicate outside of LinkedIn and your employer. You can create an anonymous username or use your real name.
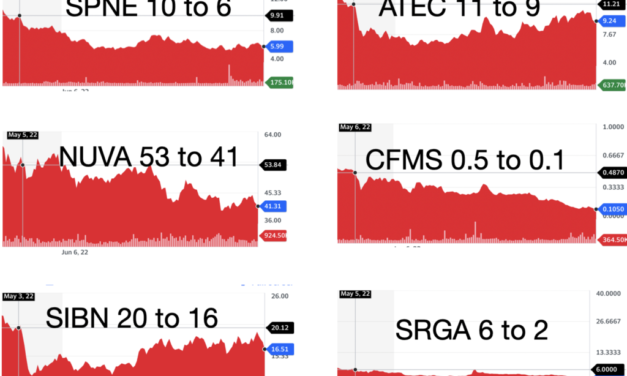
How: Use the Slack app on your mobile phone or desktop. Ask anything, share anything. Create new discussion topics inside the app (eg: NUVA+Globus).
Cost: The first “Founding Members” get in at $100/month. Your 1st month is completely free, and you can quit anytime.
The monthly cost will increase at member #51.
Privacy Note: We will never share or sell your information.
Sign up here risk free.
Read More