 Could the future of joint replacement be 3D? (Private Healthcare UK)
Could the future of joint replacement be 3D? (Private Healthcare UK)
In the UK, there are in excess of 160,000 hip and knee replacement operations performed every year and that number is just set to rise with an ever-growing aging population experiencing joint wear and tear. Contributing to a rise in overall figures also is the increase in younger patient undergoing replacement operations.
Hip replacements, usually associated with the elderly, has seen a marked rise in the younger patient. Recently released NHS data points to a 76% increase in this operation in men and women under the age of 59.
Stephen Cannon, vice president of the Royal College of Surgeons explained: “Chronic hip pain can have a devastating effect on quality of life and the ability to remain active. People don’t want to live with this pain if they can confidently undergo a hip replacement that’s successful and lasts. It’s no longer seen as a last resort.”
And it’s down in part to technological advances in hip replacements, particularly in relation to prosthetics, that is fueling this increased demand for an end to chronic hip pain in younger patients.
One size doesn’t fit all
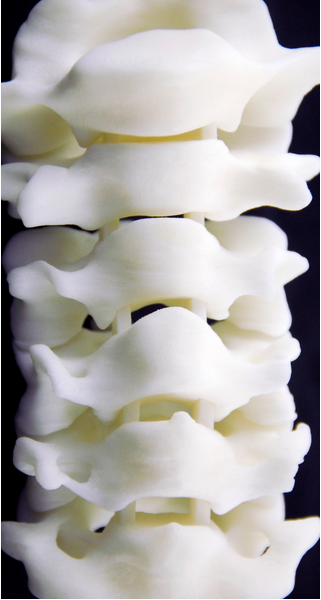
In recent years, we’ve seen the emergence of 3D-printing used in planning the operation and for patient-specific implants.
Younger patients that still want to remain fit and active, have higher expectations of the feel and function of their knee or hip replacement. Currently, there are various size prostheses available in total hip or knee replacement but shape is the same. Not only are hip and knee joints different sizes, but they are also shaped and contoured differently which is where custom-made prostheses using 3D printing is coming into its own.
Surgeons can also create hi-tech, virtual models of their patients before operating on knee and hip joints, and make the precise instruments using 3D printing technology, which could radically improve both the effectiveness of the surgery as well as reduce recovery times.
Fortius Hip Surgeon Giles Stafford, uses custom made patient specific 3D printed instrumentation and implants when it’s right for a patient. Using a 3D-printed prosthesis, allows the surgeon to fit a joint replacement that fits the knee or hip more exactly which means less bone has to be cut to fit the prosthesis. This is particularly important for a younger patient because they may require revision surgery in the future, so conserving as much bone as possible is of prime importance.
Other benefits of this type of precision joint replacement surgery, is that there is a larger surface area left for fixing the new prosthesis which typically results in a stronger and better melding of bone to implant. There is also less blood loss and the procedure can be quicker.
Further three-dimensional possibilities
Other developments in this field in recent years include the concept of scanning soldiers’ bodies in case of injury. Experts at the University of Nevada were working with the US military on the idea of creating a virtual ‘twin’ for each soldier entering the field of battle so a new bone or joint could be 3D printed in the event of injury.
Another development that was published just last month is the 3D printing of cartilage to replace the meniscus in the knee, for example, when damaged or worn down. Scientists at Duke University have developed a hydrogel-based material that is the closest to human cartilage in strength and elasticity while still being effective to use in the 3D printing process.
New advances balanced with patient safety
It is vital that new advances are balanced with patient safety and the needs of each individual case.
At the Fortius Clinic, their orthopaedic surgeons always stay abreast of the latest developments in their field and, while medical innovation is always welcomed, what’s best for the patient is of paramount importance.
Mr Marcus Bankes, hip specialist at the Fortius Clinic, explains: “Just because something is new does not mean it is better. We need at least 10 years’ data or more before we are convinced that a new material is as good as what we currently have, and the best surgeons are able to choose the right prosthesis for the right patient, and then fit it well.”